What Regulatory Compliance Governs Medical Parts?
As the world of healthcare changes quickly, strict rules must be followed when making and distributing  to protect patients and make sure the products work. Medical part makers, healthcare workers, and patients all need to understand the complicated web of rules that control these parts. These rules cover a lot of different areas, from creation and production methods to quality control and monitoring after the product has been sold. Global healthcare is always getting better, so regulatory bodies around the world are always changing and improving their rules to keep up with new technologies and health issues. This piece goes into detail about how to follow the rules when making medical parts. It talks about important governing groups, rules that must be followed, and how these rules affect the medical device business.
to protect patients and make sure the products work. Medical part makers, healthcare workers, and patients all need to understand the complicated web of rules that control these parts. These rules cover a lot of different areas, from creation and production methods to quality control and monitoring after the product has been sold. Global healthcare is always getting better, so regulatory bodies around the world are always changing and improving their rules to keep up with new technologies and health issues. This piece goes into detail about how to follow the rules when making medical parts. It talks about important governing groups, rules that must be followed, and how these rules affect the medical device business.
FDA Regulations for Medical Parts
Quality System Regulation (QSR)
The Quality System Regulation (QSR) is one of the most important FDA rules for medical parts. These detailed guidelines explain the good manufacturing practices (GMPs) that companies must follow to make sure that medical products are safe and work well. The QSR talks about many parts of the production process, like quality assurance methods, design rules, and manufacturing processes. As required by these rules, manufacturers must set up and keep up a quality control system that makes sure that medical parts are always made to meet certain standards. The QSR also talks about how important it is to handle risks and keep making the manufacturing process better. This helps keep quality and safety standards high when making medical parts.
Premarket Notification (510(k))
The 510(k) method, also known as the Premarket Notification, is an important legal route for many medical parts that want to enter the U.S. market. In this process, makers have to show that their new medical part is very similar to a gadget that is already on the market and is legal to sell. The 510(k) application must include specific information about how the gadget is designed, what it is meant to do, and how well it works. The FDA looks at this information to see if the new medical part meets the standards for safety and usefulness. This process helps make sure that new medical parts are carefully tested before they are given to patients. This balances new ideas with the safety of patients.
Medical Device Reporting (MDR)
The FDA set up Medical Device Reporting (MDR) as an important post-market monitoring method to make sure that medical parts are safe after they have been sold. This rule says that makers, suppliers, and centers that use devices must tell the FDA about certain problems and bad events that happen with their products. These reports help find possible safety problems with medical parts so that steps can be taken quickly to protect people's health. The MDR system is very important for making sure that medical parts are safe and work well throughout their whole lifetime. It does this by giving makers and regulatory bodies useful feedback.
ISO Standards for Medical Parts Manufacturing
ISO 13485: Quality Management Systems
ISO 13485 is a standard that is known all over the world and lays out the rules for a quality management system in the medical device business. The people who work for companies that develop, make, install, and fix medical items should follow this standard. It stresses how important it is to control risks and stay focused on legal requirements throughout the whole duration of a product. Manufacturers of medical parts who follow ISO 13485 show that they are dedicated to always meeting customer and governmental needs. This standard helps make sure that medical parts are made in controlled environments with the right paperwork and can be tracked back to the manufacturer. This improves patient safety and product effectiveness in the long run.
ISO 14971: Risk Management
ISO 14971 is a very important standard that describes how risk management can be used with medical devices and parts of medical devices. This standard gives companies that make medical parts a way to find, analyze, and manage the risks that come with them throughout their whole lifetime. It stresses how important it is for makers to be proactive about risk assessment and prevention methods. This helps them see and fix possible safety problems before they happen. By using ISO 14971, companies can make sure that the medical parts they make are made with patient safety in mind. This lowers the risk of problems happening and raises the quality of the products overall.
ISO 11607: Packaging for Terminally Sterilized Medical Devices
The important standard ISO 11607 talks about how to package medical parts that have been fatally cleaned. The standard makes sure that the materials and methods used to package medical parts keep the parts clean until they get to the person who will use them. Design, proof, and stable testing are some of the things that it covers when it comes to packing. Following ISO 11607 is important for companies that make medical parts that need to be sterilized because it helps the products stay intact and germ-free while they are being shipped and stored. This standard is very important for keeping medical parts safe and clean until they reach doctors and patients from being contaminated.
European Union Medical Device Regulation (EU MDR)
Classification of Medical Devices
The European Union Medical Device Regulation (EU MDR) sets up a complete method for sorting medical parts into groups based on what they are meant to do and the risks that come with it. This system, which goes from Class I (low risk) to Class III (high risk), tells us how closely we have to look at each medical part and what rules we have to follow. The process of classifying things looks at things like how long they are used, how invasive they are, and how they might affect the body. To make sure they follow the rules, manufacturers must correctly label their medical parts according to things like clinical evaluation needs and conformity assessment processes. This method of labeling helps make sure that the amount of government control is right for each medical part's possible risks.
Clinical Evaluation and Post-Market Surveillance
The EU MDR puts a lot of weight on clinical review and monitoring of medical parts after they have been sold. Manufacturers have to do detailed clinical tests on their goods to show that they are safe and work well throughout their entire lives. This includes getting and studying clinical data from different places, like clinical studies, book reviews, and experience after the product has been sold. The EU MDR also requires strong post-market monitoring methods to keep an eye on the safety and effectiveness of medical parts even after they have been sold. This ongoing monitoring helps find problems early and lets fixes be made quickly, which improves patient safety and the usefulness of the product.
Unique Device Identification (UDI) System
A key part of the EU MDR is the Unique Device Identification (UDI) system, which is meant to make it easier to track and identify medical items all along the supply chain. As part of this system, makers must give each medical part and its packaging a unique number that can be read by both humans and computers. It makes patients safer because the UDI method makes it easy to quickly and correctly identify medical parts in case of recalls or safety alerts. It also makes it easier to keep track of supplies and fights fraud in the medical equipment business. As part of the UDI standards, manufacturers must make sure that their medical parts are properly labeled and that their data is sent to the European database on medical devices (EUDAMED).
Conclusion
Ensuring the safety and effectiveness of these key parts of healthcare is very important, which is why the rules that govern them are difficult and are always changing. Manufacturers have to follow many rules and laws to get their products sold in different countries. These include FDA rules in the US, ISO standards, and the EU MDR in Europe. In the medical device business, these rules not only set high standards for quality and safety, but they also support new ideas and constant growth. Regulators will keep changing and improving their rules as technology gets better and new problems come up, so the medical parts business needs to keep working together.
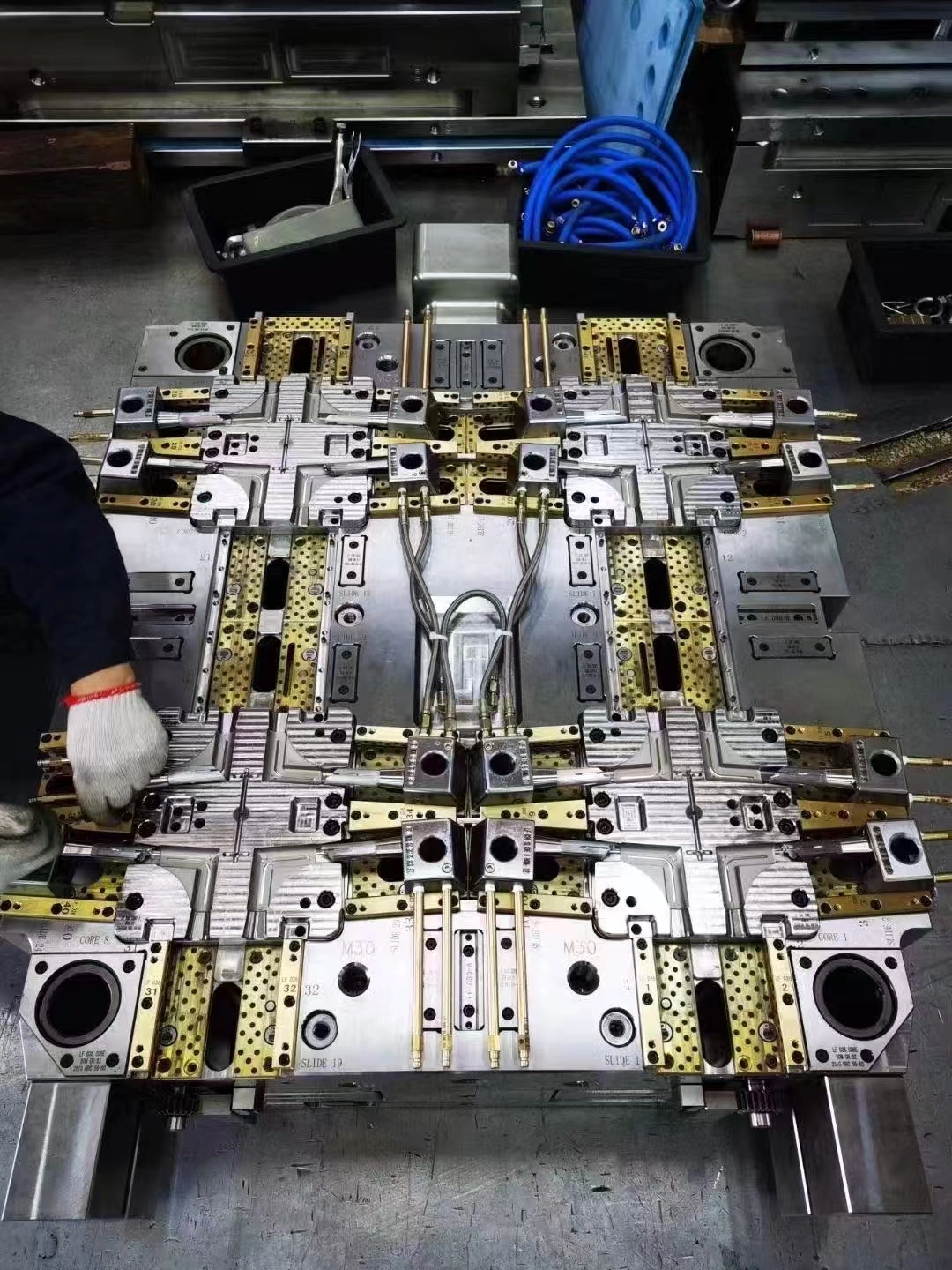
For those seeking high-quality medical parts that meet stringent regulatory standards, Alwin Asia Limited, registered in Hong Kong, offers exceptional products and services. Our manufacturing facility, Dongguan Yongsheng Hardware Plastic Product Co., Ltd., has over 20 years of experience in producing plastic molds, die-casting molds, and plastic products. Located in Changan Town, Dongguan City, Guangdong Province, we are ISO9001:2015 certified and specialize in OEM manufacturing, providing comprehensive services from design to production. Our commitment to quality, cost-effectiveness, and timely delivery makes us an ideal partner for medical parts manufacturing. For inquiries, please contact us at sales-c@alwinasia.com.
FAQ
Q: What is the main purpose of regulatory compliance for medical parts?
A: The main purpose is to ensure patient safety, product efficacy, and consistent quality in medical parts manufacturing and distribution.
Q: How often are regulatory standards for medical parts updated?
A: Regulatory standards are continuously reviewed and updated to keep pace with technological advancements and emerging health concerns.
Q: What is the difference between FDA and EU MDR regulations?
A: While both aim to ensure medical device safety, FDA regulations are specific to the U.S. market, while EU MDR applies to the European Union and has some distinct requirements, such as the UDI system.
Q: Are ISO standards mandatory for medical parts manufacturers?
A: While not always legally mandated, ISO standards are widely recognized and often required by regulatory bodies and customers as a demonstration of quality and safety.
Q: What is the importance of post-market surveillance in medical parts regulation?
A: Post-market surveillance helps identify potential safety issues after a product is on the market, allowing for timely interventions to protect public health.
References
1. U.S. Food and Drug Administration. (2021). "Medical Device Regulations and Guidance."
2. International Organization for Standardization. (2016). "ISO 13485:2016 Medical devices — Quality management systems — Requirements for regulatory purposes."
3. European Commission. (2017). "Regulation (EU) 2017/745 on medical devices."
4. World Health Organization. (2020). "Global Model Regulatory Framework for Medical Devices including in vitro diagnostic medical devices."
5. ASTM International. (2019). "Standard Guide for Characterization and Testing of Raw or Starting Materials for Tissue-Engineered Medical Products."
6. International Medical Device Regulators Forum. (2020). "Essential Principles of Safety and Performance of Medical Devices and IVD Medical Devices."

We can provide a one-stop service, including design and development, mold fabrication, production, product processing, etc.

Professional injection mold, die casting mold, plastic products OEM manufacturer